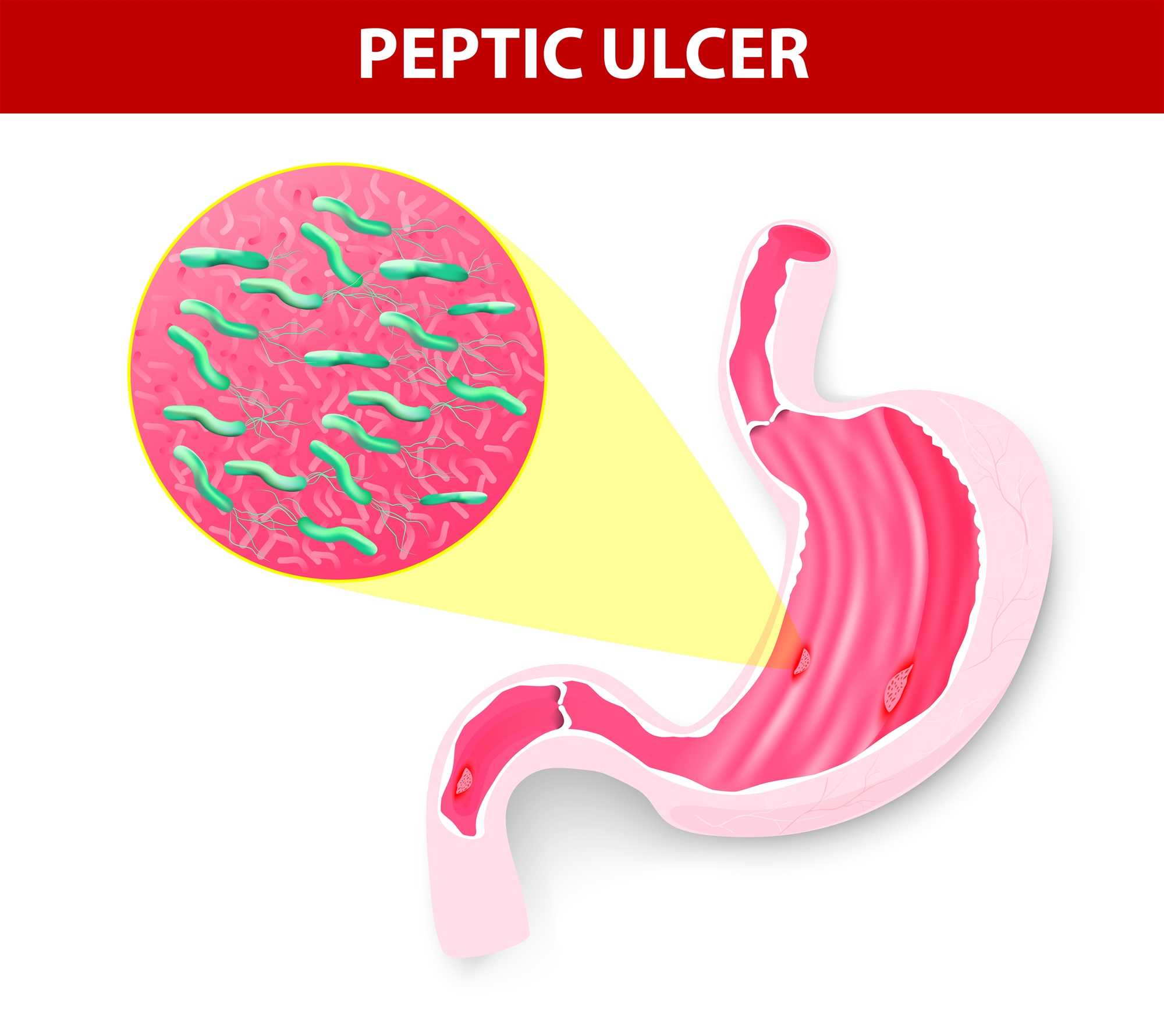
Helicobacter pylori (H. pylori) refers to the spiral bacteria with hair. Some people will not experience signs of discomfort when infected by H. pylori while others may have complications in pyloric region gastritis and doudenal ulcer due to the excess stomach acid from infection. Additionally, some people will have chronic gastritis after infected with H. pylori, which increases the risks for gastric cancer. If H. pylori can be eradicated, the probability of ulcer recurrence will drop from previous 50% to 10%.
Is therapy for H. pylori necessary?
Due to the recent popularity of health checkup in Taiwan, many people are found with H. pylori during screening but do not have the clinical symptoms, and hence they are confused if they should receive the therapy. In fact, nearly all infections with H. pylori will lead to chronic gastritis, which is the stage where most patients infected without symptoms are in. After years of development, the disease will evolve by different rate of individuals. Some people will have ulcer during the process and if they do not receive therapy for the infection, the likelihood of risk for gastric cancer or gastric lymphoma in the future will drastically increase. In view of the above, early diagnosis and early therapy should be able to prevent pathological changes in the future.
How can the patients find out if they are infected with H. pylori?
The tests for H. pylori infection can be divided into “invasive” and “non-invasive” practices.
“Invasive” practice can check if the patient is infected with H. pylori by conducting a quick urease test or histology test through endoscopic biopsy; or alternatively develop bacteria culture to understand the drug resistance against antibody.
“Non-invasive” practice generally includes three types of methods:
- C13-Urease Breath Test: Hospitals frequently adopt this test for defecting H. pylori. Patients drink C13-Urease into the stomach and if the bacteria exist, the urease will turn urea into ammonia and carbon dioxide. We can test the C13 content in the breath of patients to test the existence of H. pylori.
- Serum Antibody Test: The blood drawing test will test if there is H. pylori antigen in the serum. Patients may have been infected or are infected with H. pylori, if there is antigen in the serum. Therefore it is clinically more difficult to verify if the patients are still carriers for the bacteria when serum test is adopted, which is advised to cooperate with other tests for diagnosis.
- Stool Antigen Test: The test adopts Enzyme-Linked Immunosorbent Assay (ELISA) to detect the H. pylori antigen in stool. This method is relatively simple and safe because only stool sample needs to be collected.
What are the therapies for H. pylori?
Triple Therapy(proton pump inhibitor-PPI plus two types of antibodies) is now adopted by hospitals to eradicate H. pylori, which therapy takes 7 -14 days and can accomplish 90% effect. Nonetheless these medicines for eradicating H. pylori may cause side effects such as nausea, diarrhea, metallic taste in mouth, and allergy in few patients but these discomforts will all disappear once the patients stop taking the medicine. In 4 weeks after completing the therapy, patients usually will take breathing test to verify if H. pylori still exist. If the first-line therapy fails, we can carry out the second-line therapy using other types of antibodies based on our experience, which success rate is approximately 80%. Nonetheless if the re-eradication fails, it is advised to develop bacteria culture using endoscopic sampling in order to verify which antibodies are effective before providing suitable prescription. It is notwithstanding that there is 1% probability of recurrence or re-infection in Taiwan each year, and hence patients should pay attention to personal hygiene after successful bacteria eradication to avoid re-infection.

