The causes of diabetic retinopathy are linked to retinal hypoxia, vascular wall dysfunction, microvascular wall cell reduction, agglutination and proliferation of blood cells and platelets. Diabetic retinopathy can be divided into three categories:
- The main changes of basal diabetic retinopathy are osmotic microangioma, retinal edema, yellow hard exudates and retinal hemorrhage.
- Pre-proliferative diabetic retinopathy: When microvascular occlusion causes local retinal hypoxia and ischemia, abnormal arteriovenous aneurysms are formed, resulting in more serious leakage and bleeding.
- Proliferative diabetic retinopathy: Because of extensive retinal hypoxia, retinal neovascularization occurs, and abnormal blood vessels extend on the surface of the retina, even into the vitreous body. Once the vitreous body is pulled, it is easy to produce vitreous hemorrhage. Patients will see many plankton or spiderweb-like shadows. Repeated hemorrhage will leave blood clots blocking the vision and cause serious retinal detachment.
Examination
- Diabetics need to have fundus examination at least once a year. If there is no macular edema, patients with basal retinopathy need only have fundus examination once every six months.
- If there is significant macular edema, the fundus should be examined at least once every 3 months.
- Patients with pre-proliferative retinopathy should be examined at least once every 3 months.
- Patients with proliferative retinopathy should receive fundus follow-up examination every month.
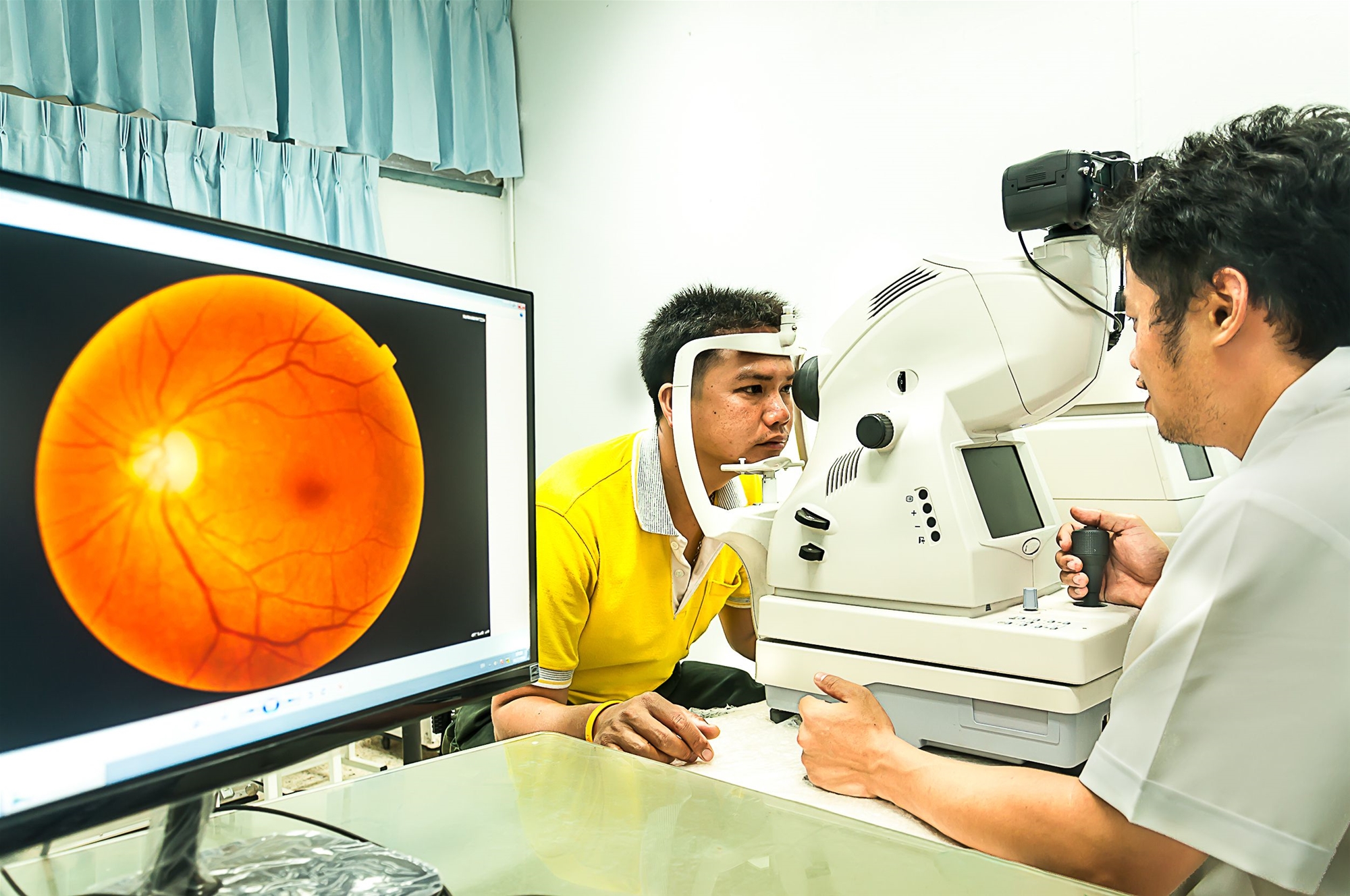
When retinopathy occurs, ophthalmoscopy can reveal marked macular edema, extensive retinal edema, or vitreous hemorrhage. If "retinal neovascularization" is suspected, fluorescent fundus photography should be arranged to detect retinopathy that is not visible under general ophthalmoscopy, so as to decide whether to receive further treatment immediately.
Diabetic retinopathy needs early examination and treatment.
Therapeutic methods
- By controlling blood sugar, blood pressure and blood fat, some blood circulation drugs can effectively alleviate part of retinal edema.
- Laser therapy can treat diabetic retinal hemorrhage and macular edema. The early stage of diabetic retinopathy can be treated by laser. Laser is a kind of concentrated strong light, which can accurately illuminate the fundus of the eye and remove the problematic blood vessels. Early laser treatment can reduce the incidence of blindness caused by retinopathy by 90 percent and prevent fluid in macular lesions from continuing to seep out of the blood vessels, but does not restore lost vision.
- Avastin intravitreal injection can reduce bleeding and inhibit abnormal vascular proliferation. Currently, the National Health Insurance program does not cover this item.
Vitrectomy is performed to treat vitreous hemorrhage and traction retinal detachment. Another cause of blindness in diabetic patients is glaucoma, which is mainly triggered by neovascularization after iris hypoxia. It grows on the iris surface and blocks the discharge of anterior chamber aqueous humor from the corner of the anterior chamber of the eye, resulting in pain and visual impairment caused by elevated intraocular pressure.

